Health
What Are Antibiotics for UTI? Types, Uses, and Effectiveness
Published
1 year agoon
By
Wilson Mark
Antibiotics for UTIs are medications designed to treat bacterial infections in the urinary tract, effectively killing or inhibiting the bacteria responsible for the infection. Choosing the right antibiotic depends on the specific bacteria involved and the severity of the infection.
Understanding UTIs and Their Impact
A urinary tract infection (UTI) occurs when bacteria invade any part of the urinary system, which includes the bladder, kidneys, ureters, and urethra.
Most UTIs affect the lower urinary tract, specifically the bladder (cystitis) and urethra (urethritis). UTIs are extremely common, particularly among women, but men, children, and older adults can also be affected.
Left untreated, these infections can lead to serious complications, such as kidney infections or sepsis.
Antibiotics are the primary treatment for UTIs, and they are effective in eradicating the bacteria responsible for the infection.
However, the choice of antibiotic depends on factors like the type of bacteria, severity, and patient’s medical history.
Symptoms of UTIs
Before diving into antibiotics, it’s important to recognize the common symptoms of UTIs.
While symptoms can vary based on the type of infection, common signs include:
- A strong, persistent urge to urinate.
- A burning sensation when urinating.
- Cloudy, dark, or bloody urine.
- Pelvic pain, especially in women.
- Foul-smelling urine.
- Fever or chills, indicating a more serious infection (such as a kidney infection).
Also Read: A Faster Way to Fat Loss: Effective Strategies for Sustainable Weight Loss
How Do Antibiotics Work for UTIs?
Antibiotics are medications that kill or inhibit the growth of bacteria.
When prescribed for UTIs, antibiotics target the bacteria responsible for the infection, most commonly Escherichia coli (E. coli), which is found in approximately 80% of cases.
Other bacteria like Klebsiella, Proteus, and Enterobacter can also cause UTIs.
The treatment duration and type of antibiotic prescribed will depend on factors such as:
- The type of bacteria causing the infection.
- The severity of the infection.
- Whether the patient has a complicated or uncomplicated UTI.
- Patient-specific factors, including allergies and medical history.
Common Antibiotics for UTIs
There are several antibiotics commonly prescribed for treating UTIs. These medications vary based on the bacteria involved, the patient’s health status, and whether the infection is uncomplicated (lower urinary tract) or complicated (involving the kidneys or recurring infections).
Nitrofurantoin (Macrobid, Macrodantin)

- Mechanism: Nitrofurantoin is an antibacterial agent that works by damaging the bacterial DNA, preventing bacterial growth and replication.
- Best for: Uncomplicated bladder infections (cystitis) caused by E. coli and other common UTI-causing bacteria.
- Advantages: Minimal bacterial resistance and suitable for short-term use.
- Not Suitable for: Patients with kidney infections or impaired kidney function.
Also Read: How and When to Avoid Alcohol: A Guide for Health and Wellness
Trimethoprim-Sulfamethoxazole (Bactrim, Septra)

- Mechanism: This antibiotic combination works by blocking the production of folic acid in bacteria, essential for bacterial survival and replication.
- Best for: Uncomplicated UTIs caused by susceptible strains of E. coli, Klebsiella, and Proteus.
- Advantages: Effective and commonly used; typically requires a 3-day treatment for uncomplicated cases.
- Resistance Issues: Increasing resistance in some regions, making it less effective in certain areas.
Fosfomycin (Monurol)
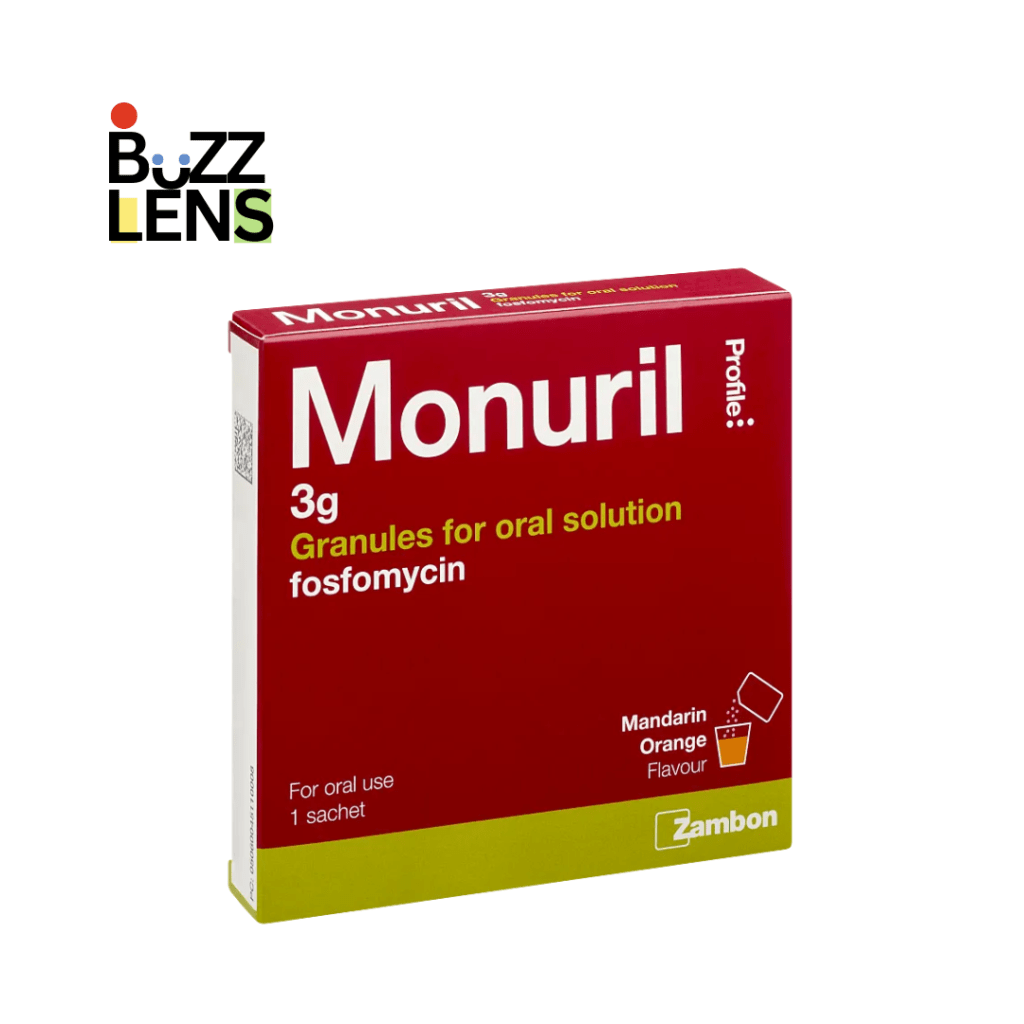
- Mechanism: Fosfomycin works by inhibiting the bacterial cell wall synthesis, preventing the bacteria from forming protective walls.
- Best for: Uncomplicated UTIs caused by E. coli and Enterococcus faecalis.
- Advantages: Given as a single-dose treatment, making it convenient for patients.
- Not Suitable for: Severe or recurrent infections, as it’s less effective in complicated UTIs.
Also Read: Understanding Anxiety Treatment: Effective Approaches and Therapies
Cephalosporins (Cefalexin, Ceftriaxone)

- Mechanism: These antibiotics target bacterial cell walls, causing them to rupture and die.
- Best for: Both uncomplicated and complicated UTIs caused by a variety of bacterial strains.
- Advantages: Broad-spectrum activity, making them useful for a wide range of infections.
- Commonly Prescribed: Cefalexin is often used for lower UTIs, while Ceftriaxone is reserved for more serious kidney infections.
Fluoroquinolones (Ciprofloxacin, Levofloxacin)

- Mechanism: These antibiotics inhibit DNA gyrase, an enzyme bacteria need to replicate DNA, stopping bacterial growth.
- Best for: Complicated UTIs, including kidney infections, caused by resistant bacteria.
- Advantages: Highly effective against a broad spectrum of bacteria.
- Warnings: Should only be used for serious infections due to potential side effects like tendon damage or nerve problems.
Also Read: Understanding the Blood Type Diet: How It Works and Its Benefits
Amoxicillin-Clavulanate (Augmentin)
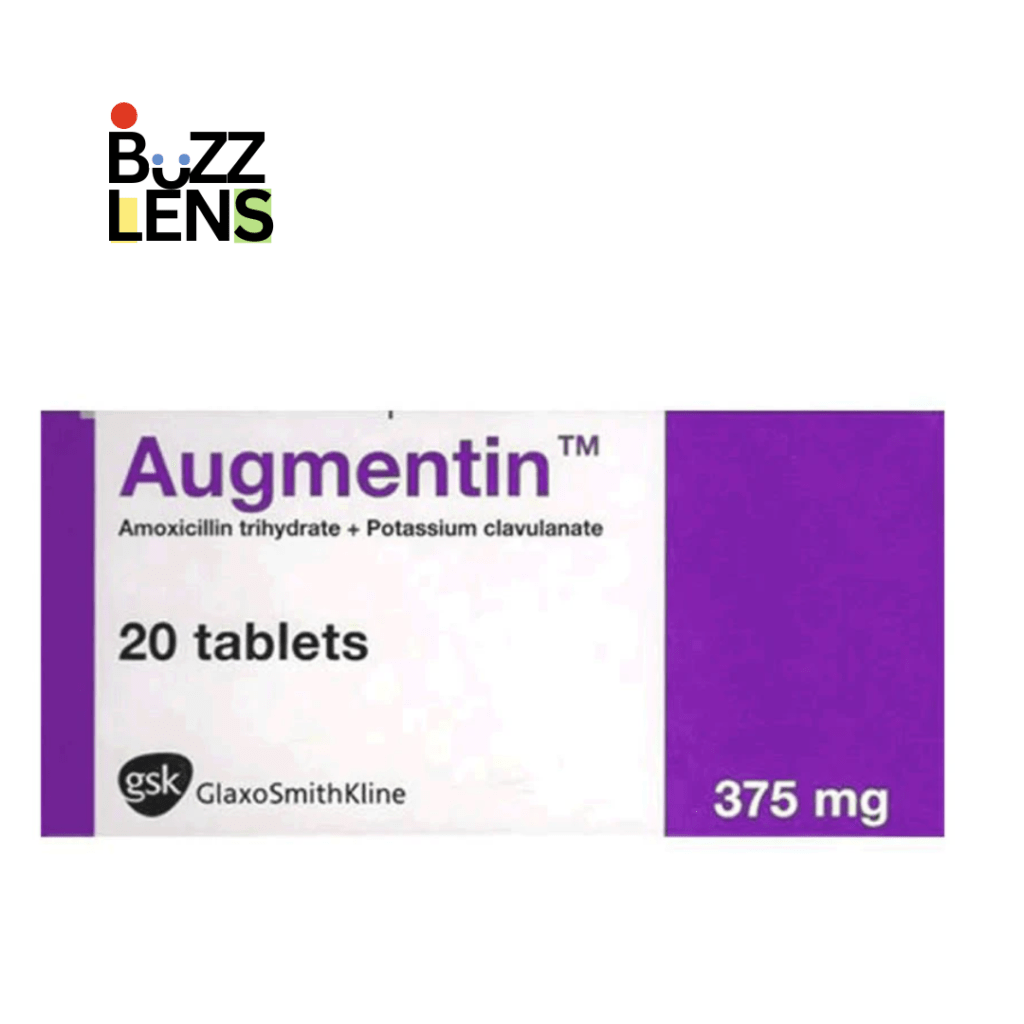
- Mechanism: This combination antibiotic inhibits bacterial cell wall synthesis and protects against beta-lactamase enzymes produced by certain resistant bacteria.
- Best for: UTIs caused by Enterococcus and Proteus species, or cases resistant to other antibiotics.
- Advantages: Broad spectrum of activity and suitable for use in children and during pregnancy.
- Not Suitable for: Patients allergic to penicillin.
Factors Influencing the Choice of Antibiotics
Type of UTI (Uncomplicated vs. Complicated)
- Uncomplicated UTIs: These are lower UTIs that occur in otherwise healthy individuals. Typically, Nitrofurantoin, Trimethoprim-Sulfamethoxazole, or Fosfomycin is prescribed.
- Complicated UTIs: These involve the upper urinary tract (kidneys) or occur in people with structural abnormalities of the urinary tract. Treatment for complicated UTIs requires stronger antibiotics, such as fluoroquinolones or cephalosporins.
Antibiotic Resistance
Due to the widespread use of antibiotics, certain bacteria have developed resistance to specific drugs. Antibiotic resistance is a growing concern worldwide, and the choice of antibiotic must consider the local resistance patterns. For instance, Trimethoprim-Sulfamethoxazole is less commonly used in areas where resistance rates are high.
Patient Factors
The patient’s age, allergies, medical history, and whether they are pregnant or breastfeeding can affect which antibiotics are safe to prescribe. Nitrofurantoin and Amoxicillin-Clavulanate are generally considered safe during pregnancy.
Duration of Antibiotic Treatment
The duration of antibiotic treatment depends on the type and severity of the UTI:
- Uncomplicated UTIs: Typically treated with a short course of 3 to 5 days.
- Complicated UTIs or Kidney Infections: May require treatment for 7 to 14 days or longer, depending on the response to the medication.
Also Read: Fiber Supplements: Boosting Digestive Health and Overall Wellness
Side Effects of Antibiotics for UTIs
While antibiotics are generally safe, they can cause side effects in some individuals.
Common side effects include:
- Nausea or vomiting.
- Diarrhea.
- Rash or allergic reactions.
- Yeast infections (due to the disruption of normal flora).
In rare cases, serious side effects such as tendonitis (from fluoroquinolones) or liver damage (from cephalosporins) may occur. It’s crucial to discuss any potential side effects with your healthcare provider.
Preventing Future UTIs
While antibiotics effectively treat UTIs, preventing future infections is key to reducing the need for antibiotics.
Tips for UTI prevention include:
- Staying hydrated: Drinking plenty of water helps flush out bacteria.
- Urinating frequently: Avoid holding urine for long periods.
- Practicing good hygiene: Wipe from front to back to prevent bacteria from spreading from the anal area.
- Cranberry supplements: Some evidence suggests that cranberry extract may help reduce the recurrence of UTIs.
Choosing the Right Antibiotic for UTI
Antibiotics are the cornerstone of treatment for urinary tract infections, and the type of antibiotic prescribed depends on factors such as the specific bacteria, severity of the infection, and patient-specific concerns like allergies or pregnancy.
It’s important to follow your doctor’s recommendations and complete the entire course of antibiotics to prevent recurrence or the development of resistant bacteria.
You may like
Health
Why Do People on Obesity Medications Drink Less Alcohol? Here’s What We Know
Published
1 year agoon
December 14, 2024By
Wilson Mark
Some people who take anti-obesity medications drink less alcohol. Scientists are trying to figure out why this happens.
How Anti-Obesity Drugs Impact Alcohol Use
Anti-obesity medications, such as Wegovy and Ozempic, may lower alcohol consumption. These drugs, called GLP-1 receptor agonists, are usually prescribed to help with weight loss and type 2 diabetes. However, new research shows they might also reduce drinking habits.
A recent study found that 45% of people on these drugs drank less alcohol. The study, published in JAMA Network Open, involved over 14,000 participants. Researchers believe this connection could lead to more discoveries about these medications.
Key Findings
Here’s what the study revealed:
- Participants: Over 14,000 individuals taking anti-obesity medications.
- Results: 45% of drinkers reduced their alcohol intake.
- Drugs Used: Medications included semaglutide, tirzepatide, and liraglutide.
- Who Benefited Most: Heavy drinkers and people with severe obesity saw the biggest change.
While most participants saw no change, only 2% drank more alcohol.
Why Do These Drugs Affect Alcohol?
The exact reason remains unclear.

However, experts have a few ideas:
- Impact on the Brain: These drugs may reduce cravings by changing how the brain processes rewards. This could lower the desire for alcohol.
- Lifestyle Changes: Many people make healthier choices while on these medications, such as eating better or drinking less.
- Lower Tolerance: Weight loss reduces alcohol tolerance, which might lead people to drink less.
More research is needed to confirm these theories.
Can These Drugs Treat Addiction?
Some experts are hopeful these drugs could help with addiction in the future. However, they are not currently approved for this use.
Dr. Timothy Brennan from Mount Sinai said, “These findings are exciting, but we need more studies to understand their effects on alcohol use.”
Researchers believe these drugs have potential, but it’s too early to draw conclusions.
Should You Avoid Alcohol While Taking These Medications?
You don’t have to stop drinking completely, but experts suggest being cautious.
Here’s why:
- Side Effects: Alcohol may worsen nausea or low blood sugar, which are common side effects of these drugs.
- Calories: Alcohol contains a lot of calories, which could slow your weight-loss progress.
- Health Benefits: Reducing alcohol may improve overall health and make the medication more effective.
If you’re starting a new medication, it’s a good time to evaluate your drinking habits.
What Should You Do?
If you’re prescribed medications like Wegovy or Ozempic, consider these tips:
- Notice if your cravings for alcohol change.
- Take this chance to build healthier habits.
- Talk to your doctor if you have concerns about drinking or other side effects.
What’s Next?
The link between anti-obesity medications and reduced drinking is fascinating. Scientists need more studies to understand how these drugs work.
For now, they remain a powerful option for weight management. The added benefit of possibly reducing alcohol consumption is an exciting bonus.
Health
How to Get Rid of Sulfur Burps: Effective Remedies and Prevention Tips
Published
1 year agoon
November 5, 2024By
Wilson Mark
Sulfur burps may be alleviated by changes in diet, proper water intake, and the use of pharmacy drugs, but it is crucial to know what causes them.
Sulfur Burps
Sulfur burps are bad-odour burps that smell like rotten eggs; many people experience this.
They can be painful and awkward and are sometimes coupled with other abdominal symptoms, including bloating, stomach-churning, or diarrhoea. The foul smell associated with sulfur burps emanates from hydrogen sulfide (H2S) generated inside your stomach.
To know how to treat and get rid of sulfur burps, it is essential to understand the causes that contribute to it.
This article will look at possible causes of sulfur burps, options for natural cure remedies, medical treatment, and ways of avoiding them.
What Causes Sulfur Burps?
Sulfur burps occur when hydrogen sulfide gas builds up in the stomach and is released through burping.

Various factors can contribute to the production of this gas, but here are the most common causes:
- Dietary Choices
Certain foods high in sulfur content can contribute to the production of sulfur gas. Some of these foods include:- Eggs
- Meat (especially red meat)
- Cruciferous vegetables like broccoli, cabbage, and cauliflower
- Garlic and onions
- Dairy products
- Beans and legumes
- Gastrointestinal Infections
Some infections, particularly those caused by bacteria like Helicobacter pylori or parasites like Giardia, can lead to sulfur burps. These infections can disrupt your digestive system, leading to excess gas production. - Indigestion or GERD (Gastroesophageal Reflux Disease)
Indigestion or GERD can slow digestion, allowing food to sit in the stomach longer and produce more gas. This gas can sometimes have a sulfurous smell, leading to sulfur burps. - Food Intolerances
Lactose intolerance, gluten sensitivity, or other food intolerances can cause incomplete digestion of food, leading to gas buildup and sulfur burps. - Medications
Some medications, particularly those containing sulfur compounds or antibiotics that affect the balance of gut bacteria, can contribute to sulfur burps.
Natural Remedies to Get Rid of Sulfur Burps
Although passing sulfur burps might be embarrassing, in most cases, they can be cured naturally. Below, I give you some home remedies that may help if you decide to try:
1. Stay Hydrated

Proper digestion requires that one drink enough water, which is determined by the intensity of the exercises. Drinking fluids eliminates accumulated toxins, thus ensuring the digestive system is working properly, and there is less likelihood of developing gas. Avoid sulfur burps by taking at least eight glasses of water per day.
2. Green Tea or Herbal Teas

Green tea, mint, or chamomile will also relax your tummy and reduce gas formation. Green tea, in particular, has antioxidants that can help with digestion, while peppermint helps to relax the gut.
3. Eat Smaller, More Frequent Meals

Eating large meals or taking more than necessary also puts pressure on the digestive system, resulting in information of gases, including sulfur. Dividing the portions into smaller meals that are taken frequently ensures that the body can break down the food into Sulphur without experiencing sulfur burps.
4. Avoid Sulfur-Rich Foods
If you experience sulfur burps often, you should reduce the intake of sulfur-containing foods such as eggs, broccoli, garlic, and dairy products. These foods may cause more gas production; therefore, cutting down or eliminating these foods from the diet may greatly help.
5. Try Apple Cider Vinegar

Apple cider vinegar (ACV) is one of the go-to home remedies for enhancing digestion. ACV has an impact on balancing the level of acidity in the stomach, hence facilitating the digestion of foods and decreasing the formation of sulfur gas. Ingest a glass of water mixed with 1 tablespoon of ACV, and see if it is taken before meals.
6. Use Probiotics
Probiotics are beneficial bacteria that promote healthy digestion by balancing the gut’s bacterial environment. Taking a probiotic supplement or eating probiotic-rich foods like yogurt, kefir, or sauerkraut can help prevent sulfur burps by keeping your digestive system balanced.
Over-the-Counter Remedies for Sulfur Burps
Several over-the-counter treatments are available if natural remedies aren’t enough to resolve your sulfur burps.
1. Antacids

Many recipes warn about foods that produce gas, but antacids can help neutralize stomach acid and leave your digestive system to do the work. This may be useful, especially if the sulfur burps originate from indigestion or GERD.
Table: Best OTC Medications for Sulfur Burps
| Medication Type | How It Helps | Example Products |
|---|---|---|
| Antacids | Neutralize stomach acid | Tums, Rolaids |
| Simethicone | Breaks up gas bubbles in the stomach | Gas-X, Mylanta Gas |
| Probiotics | Supports gut health | Culturelle, Align, Florastor |
2. Simethicone
It is an anti-gas drug that alters the sizes and distribution of gas in the stomach and intestines, promoting gas release without the smell.

Simethicone-containing products such as Gas-X or Mylanta Gas quickly relieve such pain.
3. Activated Charcoal
Charcoal is effective in absorbing gases and toxins in your stomach. The common formulation is a pill that can successfully minimize normal gas and sulfur-related burps.
Always check with your doctor before using charcoal supplements, as they may interfere with medications.
When to See a Doctor for Sulfur Burps
While sulfur burps are often harmless, they can sometimes signal an underlying health issue that requires medical attention.
If your sulfur burps are persistent or accompanied by other symptoms, such as severe abdominal pain, diarrhoea, nausea, or vomiting, it’s time to consult a doctor.
Here are a few conditions that may require medical evaluation:
1. Gastrointestinal Infections
As mentioned earlier, infections like H. pylori or Giardia can cause sulfur burps and other symptoms like bloating, nausea, diarrhoea, and stomach cramps. Testing for these conditions often involves stool, blood, or breath tests.
2. GERD or Chronic Indigestion
GERD or chronic indigestion can lead to frequent sulfur burps due to slowed digestion. If you experience heartburn, regurgitation, or pain after eating, consult a healthcare provider for proper diagnosis and treatment.
3. Food Intolerances or Sensitivities
Food intolerances, such as lactose intolerance or celiac disease, may cause sulfur burps. Your doctor may recommend elimination diets or tests to identify specific food triggers.
Prevention Tips: How to Stop Sulfur Burps from Coming Back
Once you’ve gotten rid of sulfur burps, preventing them from returning is essential. Here are some long-term strategies you can follow:
1. Monitor Your Diet
Pay attention to how certain foods affect your digestive system. Keeping a food diary can help you identify which foods trigger your sulfur burps so that you can adjust your diet accordingly.
2. Eat Slowly and Chew Thoroughly
Eating too quickly can cause you to swallow air, leading to gas and burping. Chewing food thoroughly helps your digestive system break down food more efficiently, reducing the chance of sulfur gas forming.
3. Avoid Carbonated Beverages
Carbonated drinks like soda and sparkling water introduce extra air into your stomach, which can lead to burping. Try to cut down on these beverages to reduce gas and sulfur burps.
4. Exercise Regularly
Regular physical activity can improve digestion by keeping things moving through your gastrointestinal tract. Even light activities like walking after a meal can help prevent gas buildup.
5. Stay Hydrated
Hydration is vital to maintaining healthy digestion. Water helps break down food and keeps things moving through your digestive system, reducing the likelihood of gas formation.
Banish Sulfur Burps for Good
Sulfur burps may be unpleasant, but they’re usually treatable with dietary changes, natural remedies, and over-the-counter medications.
Whether you’re dealing with a one-time issue or chronic sulfur burps, identifying the underlying cause is the first step toward relief.
By adjusting your diet, staying hydrated, and trying some of the remedies outlined here, you can eliminate sulfur burps and prevent them from returning.
Remember, if sulfur burps persist or are accompanied by other severe symptoms, it’s essential to consult a healthcare provider to rule out any underlying health issues.
Health
Mens Mental Health Month: When It Is and Why It Matters
Published
1 year agoon
October 6, 2024By
Wilson Mark
Men’s Mental Health Month is observed in November, raising awareness about the unique mental health challenges men face and encouraging open discussions on emotional well-being.
The Importance of Mens Mental Health
Mental health affects everyone, but the stigma surrounding men’s mental health often prevents open conversations about emotional well-being.
In recognition of these challenges, Men’s Mental Health Month is observed each year in November to promote awareness, break the stigma, and encourage men to seek help when needed.
Mental health conditions can affect men of all ages, and during this month, the focus is on addressing the barriers men face in receiving the care and support they need.
This article will delve into the significance of Mens Mental Health Month, explore the mental health struggles specific to men, and provide resources for those looking to improve their well-being.
Why Is November Mens Mental Health Month?
November was chosen as Mens Mental Health Month to align with Movember, a global movement that encourages men to grow mustaches to raise awareness of men’s health issues, including mental health, prostate cancer, and testicular cancer.

The month-long campaign focuses on mental health as one of its core pillars, promoting open conversations about depression, anxiety, and suicide prevention.
The goal is to highlight the importance of mental well-being and reduce the stigma that often surrounds it for men.
Also Read: Understanding Anxiety Treatment: Effective Approaches and Therapies
The Mental Health Crisis Among Men
Men’s mental health is an often-overlooked area of public health, despite the fact that men are disproportionately affected by certain mental health issues.
Understanding the unique pressures men face is critical to promoting effective treatment and support.
Statistics on Men’s Mental Health
- Depression: Over 6 million men in the U.S. are affected by depression every year, but men are less likely to seek help for it compared to women.
- Suicide: Men die by suicide at a rate 3.88 times higher than women in the U.S., according to the American Foundation for Suicide Prevention.
- Substance Abuse: Men are more likely to turn to substance abuse as a way to cope with mental health issues. Approximately 20% of men are affected by alcohol dependency at some point in their lives.
Table 1: Key Statistics on Men’s Mental Health
| Mental Health Condition | Percentage of Men Affected | Impact |
|---|---|---|
| Depression | 6 million men in the U.S. | Lower rates of seeking help, higher risk of untreated symptoms |
| Suicide | Men 3.88 times more likely than women | Often linked to untreated mental health issues |
| Substance Abuse | 20% of men experience alcohol dependency | Often a coping mechanism for untreated mental health issues |
Why Men Don’t Seek Help: Breaking the Stigma
One of the core issues behind men’s mental health challenges is the stigma attached to seeking help. Many men grow up with societal pressures to appear strong, unemotional, and independent.
These cultural norms can make it harder for men to admit they are struggling or to seek therapy and other mental health resources.
Cultural Expectations and Toxic Masculinity
Toxic masculinity refers to the societal expectation that men should suppress emotions, avoid vulnerability, and never ask for help.
While not all traditional masculine traits are harmful, those rooted in the idea that men should never show weakness can be damaging.
This mindset often leads to men ignoring their mental health needs, resulting in long-term issues that can worsen over time.
Barriers to Seeking Help
- Fear of Judgment: Many men avoid seeking help for fear of being judged as weak or incapable.
- Lack of Awareness: Some men may not recognize the signs of mental health issues or may attribute their symptoms to physical illness rather than emotional distress.
- Accessibility: Access to affordable mental health care is another barrier, particularly in areas where resources are limited.
Also Read: Understanding the Silent Epidemic of Suicide: Key Insights for World Suicide Prevention Day
The Role of Mens Mental Health Month in Breaking the Stigma
Men’s Mental Health Month aims to break down the stigma surrounding mental health by promoting open conversations about emotional well-being and providing resources for those in need.

The month serves as a platform for spreading awareness about the prevalence of mental health conditions among men and educating the public on the importance of seeking help.
Key Initiatives During Mens Mental Health Month
- Movember Campaign: As part of Movember, men around the world grow mustaches in November to raise awareness of men’s health issues, including mental health. The movement encourages conversations about mental well-being and offers support through its fundraising initiatives.
- Mental Health Screenings: Various mental health organizations promote free or low-cost mental health screenings during the month to help men identify early symptoms of depression, anxiety, and other conditions.
- Social Media Campaigns: Platforms like Twitter and Instagram play a significant role in spreading awareness. Hashtags such as #MensMentalHealth and #Movember are used to promote the cause and encourage men to share their stories.
Mental Health Conditions Common Among Men
While mental health challenges affect all genders, certain conditions are more prevalent among men or manifest differently in men compared to women.
During Mens Mental Health Month, it’s essential to shine a light on these issues.
Depression in Men
Depression in men often goes unnoticed because it can manifest differently compared to women.
While women may experience feelings of sadness and hopelessness, men are more likely to exhibit symptoms such as irritability, anger, and fatigue.
Men may also be more likely to distract themselves from their depression through substance abuse or overwork.
- Symptoms of Male Depression: Anger, irritability, loss of interest in hobbies, fatigue, difficulty concentrating, and physical symptoms such as headaches or digestive problems.
- Coping Mechanisms: Men may turn to harmful behaviors like excessive drinking or substance abuse to numb their emotions rather than seeking therapy or counseling.
Anxiety in Men
Anxiety is another common mental health issue that affects men. It often goes hand-in-hand with depression and can manifest as excessive worrying, panic attacks, or social withdrawal.
- Common Triggers for Anxiety in Men: Job stress, financial pressures, relationship challenges, and societal expectations.
- Physical Symptoms: Anxiety in men can lead to physical symptoms like muscle tension, heart palpitations, or trouble sleeping.
Substance Abuse and Mental Health
Men are more likely than women to cope with mental health issues by turning to alcohol or drugs.
While this may temporarily relieve symptoms of depression or anxiety, substance abuse often worsens mental health in the long run and can lead to dependency.
Table 2: Common Mental Health Conditions Among Men
| Condition | Symptoms in Men | Prevalence |
|---|---|---|
| Depression | Anger, irritability, fatigue | 6 million U.S. men |
| Anxiety | Excessive worry, panic attacks, social withdrawal | Affects 1 in 10 men |
| Substance Abuse | Heavy drinking, drug use | 20% of men experience alcohol dependency |
Ways to Improve Mens Mental Health
There are several steps men can take to improve their mental health and well-being. Men’s Mental Health Month is the perfect time to start making small changes that can have a big impact.
1. Talk About It
One of the most powerful ways to combat mental health stigma is to talk about it. Whether it’s opening up to a friend or family member, joining a support group, or even posting on social media, talking about mental health can help break the stigma.
2. Seek Professional Help
Therapists and counselors are trained to help individuals manage their mental health challenges. Seeking professional help isn’t a sign of weakness—it’s a proactive step toward better well-being. Therapy can provide men with the tools they need to navigate their emotions and cope with life’s challenges in a healthy way.
3. Practice Self-Care
Taking care of your mental health requires practicing self-care, such as getting regular exercise, maintaining a healthy diet, and making time for activities that bring joy. Self-care doesn’t have to be complicated—it can be as simple as going for a walk, practicing mindfulness, or spending time with loved ones.
4. Join a Community
For many men, finding a supportive community can make a big difference. Whether it’s through an online forum, a local support group, or a sports team, connecting with others who understand and share similar experiences can reduce feelings of isolation.
Also Read: What Is Stockholm Syndrome? Understanding the Psychological Phenomenon
How to Support Mens Mental Health Year-Round
While Men’s Mental Health Month is observed in November, it’s important to support men’s mental health year-round.
Encouraging men to seek help, promoting open conversations about mental health, and advocating for accessible resources are essential steps in improving the mental well-being of men everywhere.
Table 3: Year-Round Strategies to Support Men’s Mental Health
| Strategy | Action |
|---|---|
| Promote open conversations | Encourage men to talk about their emotions and mental health struggles without fear of judgment. |
| Advocate for mental health resources | Support policies and organizations that make mental health care more accessible. |
| Encourage self-care | Remind men to prioritize their mental well-being through regular self-care practices. |
| Build supportive communities | Create spaces where men feel safe to share their experiences and challenges. |
Mens Mental Health Matters
Men’s Mental Health Month in November serves as a critical time to raise awareness about the unique mental health challenges that men face.
By addressing the stigma around seeking help, promoting open conversations, and providing resources, we can make strides in improving the mental well-being of men.
Mental health is an essential part of overall well-being, and men must feel empowered to seek help, take care of themselves, and prioritize their emotional health.
This November, take the time to support the men in your life by encouraging open conversations about mental health, promoting self-care, and advocating for greater access to mental health resources.
With collective effort, we can reduce the stigma and ensure that men receive the support they need.

iOS 26 Explained: Stability & The Future of iPhones
Magnitude 5.1 Earthquake Rattles Northern Iran — No Major Damage Reported

Why Do People on Obesity Medications Drink Less Alcohol? Here’s What We Know
Trending
-

 FASHION9 years ago
FASHION9 years agoThese ’90s fashion trends are making a comeback in 2017
-

 Entertainment9 years ago
Entertainment9 years agoThe final 6 ‘Game of Thrones’ episodes might feel like a full season
-

 FASHION9 years ago
FASHION9 years agoAccording to Dior Couture, this taboo fashion accessory is back
-

 Entertainment9 years ago
Entertainment9 years agoDisney’s live-action Aladdin finally finds its stars
-

 Entertainment9 years ago
Entertainment9 years agoThe old and New Edition cast comes together to perform
-

 Sports9 years ago
Sports9 years agoPhillies’ Aaron Altherr makes mind-boggling barehanded play
-

 Sports9 years ago
Sports9 years agoBoxing continues to knock itself out with bewildering, incorrect decisions
-

 Sports9 years ago
Sports9 years agoSteph Curry finally got the contract he deserves from the Warriors